Radiation reduction is a top quality metric for improving patient outcomes. One example can be seen with the HCA system and their Radiation Right program. This program promotes considering alternative exams that can still meet the patient needs while minimizing exposure to ionizing radiation. Choosing Wisely® and the Centers for Medicare and Medicaid (CMS) also have initiatives to reduce radiation exposure. These initiatives are specifically aimed at reducing radiation in the mild head injured patient population, as over 80% of these patients receive a head CT with over 90% of the results negative for a brain bleed.
Given that 3.6% of all ED visits present for head injury, there is significant opportunity to improve the value of care for ED patients.1Head CTs that expose patients to ionizing radiation and can increase a patients’ lifetime risk of cancer should not be performed when clinicians can safely risk stratify a patient without the expense of a potentially harmful test.2 The current risk stratification practice is the use of clinical decision rules (CDRs) – Canadian Head CT Rule, New Orleans Criteria, and/or Nexus II.
Despite these radiation reduction initatives, many Emergency Clinicians report performing low-value services, such as CT in minor head injury.3 In the case of a head CT, Emergency Clinicians cited “concern for serious diagnosis” or “patient or family expectations” as reasons for why they did not adhere to clinical guidelines. One of the first published evaluations was a retrospective cohort study at an academic Level-1 Trauma Center. The study included 489 patients with minor head injury and assessed whether ED clinicians appropriately applied the Choosing Wisely criteria. The NEXUS II clinical decision rule, which uses a series of clinical criteria to risk stratify the severity of a patient’s head injury, was used as a benchmark.4 Clinicians captured the clinical criteria for the decision rule well; however, they still obtained “non-indicated” CTs in 23.1% of patients.5
Integration of BrainScope could help providers and hospitals more reliably meet their quality initiatives, address concern for serious diagnosis and meet patient/family expectations by giving them an objective point of care decision support tool. BrainScope has demonstrated a 99% sensitivity in identifying the likelihood of the smallest detectable level of intracranial blood (>1 mL) in patients with minor head injury.6 Using objective, AI-derived algorithms BrainScope provides Emergency Clinicians with both the likelihood of having an intracranial hemorrhage and a brain function impairment such as concussion after a minor head injury. These measures give both clinicians and their patientss objective information related to their head trauma without subjecting them to ionizing radiation.
BrainScope can be integrated into the use of the CDRs improving the overall reduction of low value head CTs. The diagram below shows the potential impact to head CT utilization for 100 patients. In this example, the integration of BrainScope increases the reduction of low value head CTs from 22% (CCHR only) to 46%.
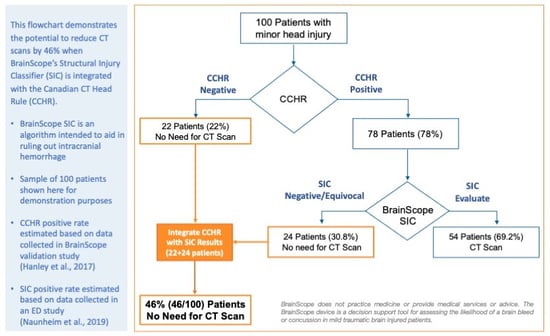
To demonstrate this further, in a 40,000 visit/year emergency deparment with 1,000 mild head injured patients, integration of BrainScope could lead to an additional 230 patients in compliance with quality metrics. Further, use of BrainScope can decrease ED LOS associated with a CT scan, reduce total healthcare costs for payers and patients, improve ED patient satisfaction, and provide a brain function assessment to objectively discuss a patient’s prognosis and arrange appropriate follow-up.
Read Next: Toward a Better Care Pathway for Minor Head Injury
1. Korley, F. K., Kelen, G. D., Jones, C. M., & Diaz-Arrastia, R. (2016). Emergency department evaluation of traumatic brain injury in the United States, 2009–2010. The Journal of head trauma rehabilitation, 31(6), 379.
2. Avoid computed tomography (CT) scans of the head in emergency department patients with minor head injury who are at low risk based on validated decision (Choosing Wisely) rules.https://www.choosingwisely.org/clinician-lists/american-college-emergency-physicians-ct-scans-of-head-for-emergency-department-patients-with-minor-head-injury/ (accessed Sept 30, 2022).
2. Lin, M. P., Nguyen, T., Probst, M. A., Richardson, L. D., & Schuur, J. D. (2017). Emergency physician knowledge, attitudes, and behavior regarding ACEP's choosing wisely recommendations: a survey study. Academic Emergency Medicine, 24(6), 668-675.
3. Mower, W. R., Hoffman, J. R., Herbert, M., Wolfson, A. B., Pollack Jr, C. V., Zucker, M. I., & NEXUS II Investigators. (2002). Developing a clinical decision instrument to rule out intracranial injuries in patients with minor head trauma: methodology of the NEXUS II investigation. Annals of emergency medicine, 40(5), 505-515.
4. Raja, A. S., Venkatesh, A. K., Mick, N., Zabbo, C. P., Hasegawa, K., Espinola, J. A., ... & Camargo Jr, C. A. (2017). “Choosing Wisely” imaging recommendations: initial implementation in New England emergency departments. Western Journal of Emergency Medicine, 18(3), 454.
5. Hanley, D., Prichep, L. S., Bazarian, J., Huff, J. S., Naunheim, R., Garrett, J., ... & Hack, D. C. (2017). Emergency department triage of traumatic head injury using a brain electrical activity biomarker: a multisite prospective observational validation trial. Academic emergency medicine, 24(5), 617-627.