When patients arrive at the emergency department (ED) with a suspected head injury, clinicians need to quickly assess for severity and determine next steps. Does the patient have a brain injury—brain bleed, concussion, or both? Understanding what happens to the brain following a head injury can help determine the next steps for assessment and treatment.
A traumatic brain injury (TBI) can be caused by a bump, blow, jolt to the head, or penetrating head injury. When a TBI occurs, the brain is pushed against the inside of the skull at various speeds, causing sheering forces that can stretch and tear nerve tissue. This imbalance of ions and chemicals can impair nerve cell function potentially decreasing communication between different brain regions or causing a bleed in the brain tissue.
TBI can result in a cascade of brain injury, typically in two phases.
The initial phase of injury is induced by a mechanical force and occurs at the moment of injury. It is due to the acceleration and deceleration of the head when an object strikes the brain or the brain strikes the inside of the skull causing an intracranial hematoma, vascular injury, or injury to cranial neurons. The secondary phase can occur hours or days after trauma and can be caused by impairment in cerebral blood flow, resulting in edema, hemorrhage, or increased intracranial pressure.
Structural and functional injuries occur during a TBI but do not always complement each other. A structural injury, or acute intracranial pathology, often includes intracranial hemorrhage, cerebral edema, or contusion. A functional injury can disrupt neurochemical and metabolic function within the brain cells and can include microstructural (axonal) injury, making it more difficult for cells to function and communicate.
TBIs are classified as severe, moderate, and mild. Assessment tools, such as the Glasgow Coma Scale (GCS) are commonly used to help determine the severity of a TBI:
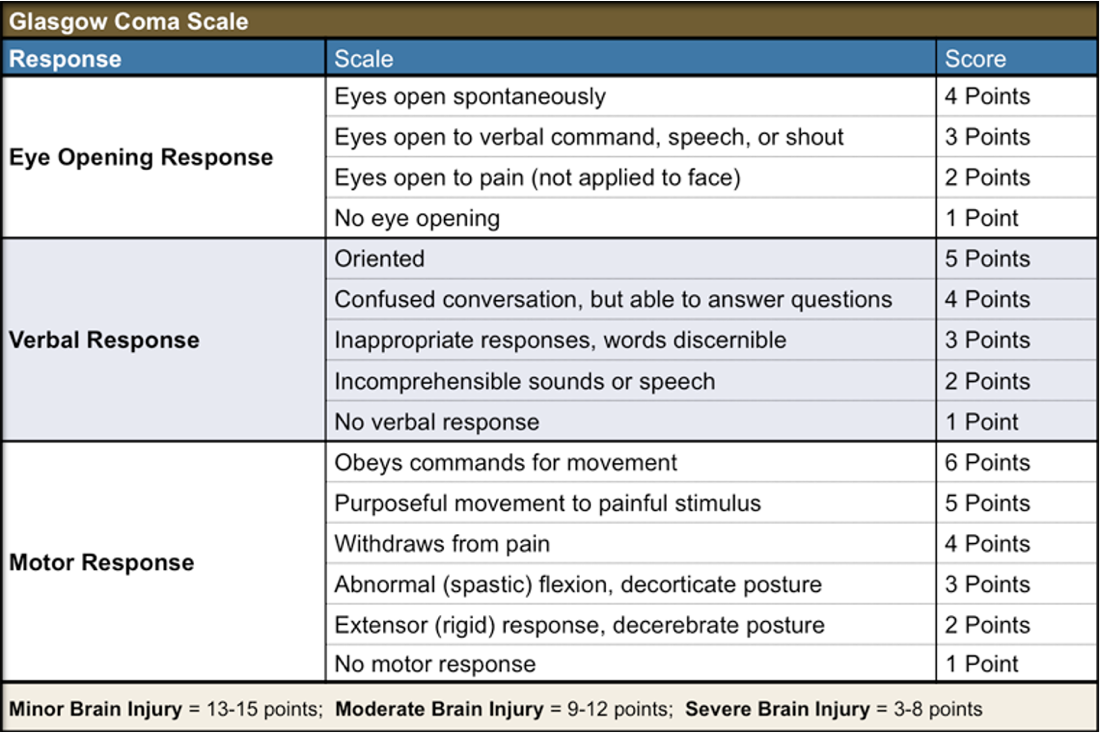
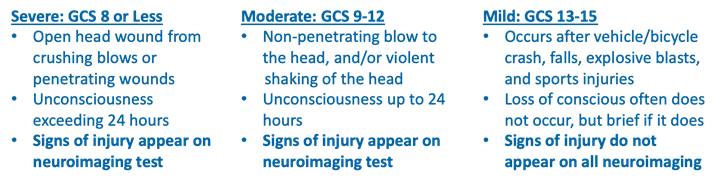
95% of head injuries seen in the ED are classified as mild traumatic brain injuries (mTBIs), with a GCS of 13-15. They are considered “mild” because most are not life-threatening. Although mTBI is often used synonymously with a concussion, mTBI patients may have a structural brain injury, a functional brain injury, or both.
Assessing and determining treatment options for mTBIs is challenging because signs of injury may not always be visible. Most commonly caused by falls, strikes by or against an object, motor vehicle accidents (MVA) or bike accidents, sports injuries, or explosive blasts. mTBI symptoms may range from mild to severe and include one or more of the following:
- Alterations in vision or hearing (sensitivity to light or sound)
- Confusion
- Feeling in a “fog”
- Drowsiness
- Disorientation
- Balance/Dizziness problems
- A sense of having lost time
- Headaches
- Loss of consciousness at time of injury
- Memory loss (amnesia) of events before the incident or immediately after
- Nausea and/or vomiting
Emergency Department clinicians are often the first line of support for head-injured patients. Standard protocols may not provide clinicians with an accurate and objective assessment.
Learn how BrainScope can help objectively triage your head-injured patients.
