As the world enters year three of COVID-19, patients are returning to the Emergency Department (ED), with volumes approaching pre-pandemic levels. Among those returning are head-injured patients—an ED patient population that has increased 30% in recent years. Seventy percent of these patients are evaluated as treat and release, but many spend up to six hours in the ED because of typical assessment protocols.
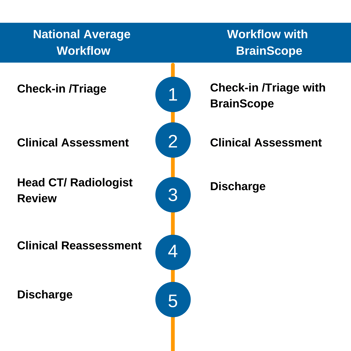
Standard protocols are often the path of least resistance in the fast-paced ED environment, even if they do result in lengthy patient visits. The head CT, the standard diagnostic tool for head injuries, provides assurance to clinicians and patients on the presence of a brain bleed. The scan takes about 20 minutes, but there is typically a long queue which is a primary cause for the patient’s length of stay and further delays related to receiving results. The image below adapted from ED Time Course for Mild Traumatic Brain Injury by Michelson and colleagues depicts the typical workflow and time for a head-injured patient receiving a head CT.
.png?width=351&name=National%20Average%20Workflow%20v1%20(1).png)
The study that produced this workflow was published in 2018. Therefore, it doesn’t account for the challenges of the current COVID-19 climate and increased ED patient volume.
Removing patients from the CT queue when a head CT is deemed not necessary can improve patient throughput, as well as align with initiatives from leading organizations such as ACEP’s Choosing Wisely. Tools such as the Canadian CT Head Rule (CCHR) and New Orleans Criteria (NOC) are decision rules intended to help clinicians determine when a patient does require a head CT. Studies have shown that the CCHR can reduce CT utilization by up to 30% when used appropriately. In general, these rules are reported to have high sensitivity at the expense of poor specificity. One study of these tools conducted in twelve EDs showed a 13% increase in CT utilization. The authors determined that several factors such as physician compliance and ED overcrowding contributed to the increase in CT utilization.
BrainScope gives clinicians an objective decision support tool to quickly triage their head-injured patients and aid in the reduction of unnecessary head CTs. In 20 minutes or less, clinicians have actionable results on the likelihood of a brain bleed and the presence and severity of concussion at the point of care. The image below contrasts the typical workflow studied in the Michelson and colleagues’ article with the BrainScope workflow.
The EEG-based assessment has a sensitivity of 99% to 1cc blood giving clinicians assurance that when a BrainScope negative result is returned, it can add confidence to removing the patient from the CT queue. The same assessment also provides a measure of the likelihood of concussion and severity. This allows clinicians to spend more time discussing the next steps with their patients, providing informed referrals when necessary, and contributing to reducing ED over-crowding in this time of COVID.
